
Am I experiencing trauma?
Trauma is not always easily recognizable in ourselves. How do we spot when we may be seeing or having a traumatic reaction?

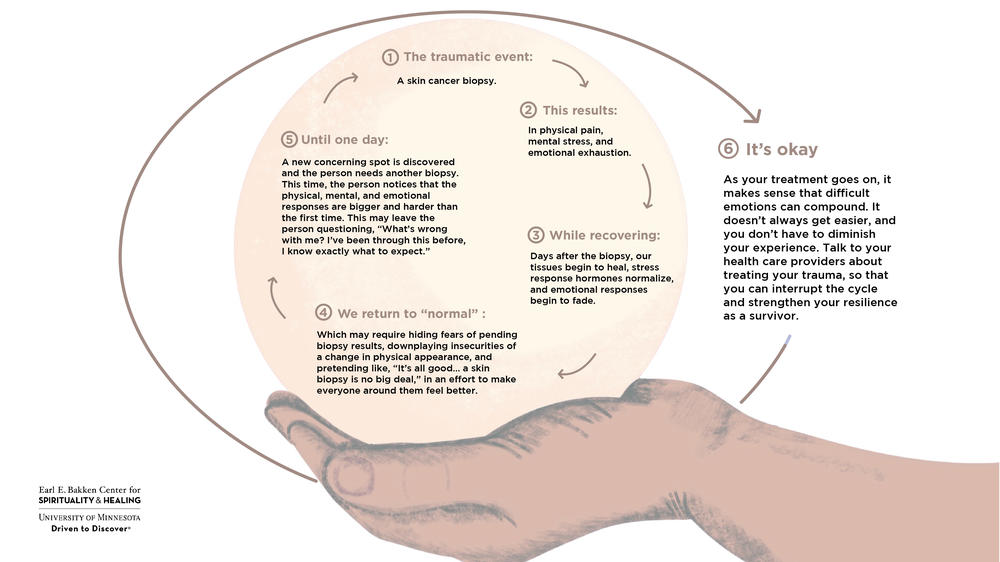
The traumatic event: a skin cancer biopsy.
This results in physical pain, mental stress, and emotional exhaustion.
While recovering days after the biopsy, our tissues begin to heal, stress response hormones normalize, and emotional responses begin to fade.
We return to “normal,” which may require hiding fears of pending biopsy results, downplaying insecurities of a change in physical appearance, and pretending like, “It’s all good… a skin biopsy is no big deal,” in an effort to make everyone around them feel better.
Until one day, a new concerning spot is discovered and the person needs another biopsy. This time, the person notices that the physical, mental, and emotional responses are bigger and harder than the first time. This may leave the person questioning, “What’s wrong with me? I’ve been through this before, I know exactly what to expect.”
It’s okay. As your treatment goes on, it makes sense that difficult emotions can compound. It doesn’t always get easier, and you don’t have to diminish your experience. Talk to your health care providers about treating your trauma, so that you can interrupt the cycle and strengthen your resilience as a survivor.
“Trauma reactions are incredibly boundaryless, so sometimes instead we try to control everything else”
There are more clues you may be seeing or having a traumatic reaction which include denial or minimization, uncontrolled anxiety or hypervigilance, and desperate attempts to control one's environment and everyone in it.
Often when we're discussing controversial topics like politics, some may show traumatic reactions through knee jerk opposition. Notably if it’s one specific issue that triggers someone to shut down or become unreasonable to debate, that can be a sign of trauma.
We do need to be upset and outraged by a lot going on, but if there’s one thing that is particularly aggravating then it’s worth recognizing, “Maybe there’s a little bit of trauma there. I wonder what that is about. How does this impact my life and relationships with others?”
A person may have a traumatizing experience without developing PTSD. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) outlines the symptoms that must be present for a diagnosis of PTSD. These are true for children over the age of 6 and adults. Often, PTSD related to medical trauma is missed or not diagnosed. This may be because healthcare teams are focused on caring for physical health diagnoses and forget to look for or ask about mental health diagnoses. Additionally, your healthcare team may not know enough about PTSD to bring it up, or how to help you if you screen positive for it. Consider the following symptoms that are present in a person with PTSD. If you think you might have PTSD, one way to start that conversation with your healthcare team is to print this PTSD screener, fill it out, and take it to your next appointment. It can be the first step in getting help for your trauma. Remember, you don’t have to qualify for a full PTSD diagnosis in order to get help.
If you have experienced any amount of trauma, mental health services can help decrease your symptoms and improve your quality of life. The Veterans Administration has some of the best developed tools for helping with PTSD. Though medical trauma is different from war trauma, there are many similarities. To learn more about PTSD and to explore additional resources for you and your family, check out the National Center for PTSD.
A person must have exposure to trauma in ONE of the following ways:
A person must also have ONE or more of the following symptoms that feels related to the traumatic event and begins after the event:
A person must have the desire to avoid things associated with the traumatic event. This often results in either or both of the following:
A person must have negative changes in mood and thoughts because of the traumatic event(s). These changes in mood must start or worsen after the traumatic event(s). A person must experience at least TWO of the following:
Ongoing negative emotional state:
A person must also have changes in their behavior and the way they react to certain things associated with the trauma. A person must experience TWO of the following:
For a diagnosis of PTSD, the symptoms described above must last more than one month. They must cause distress that is significant or impair functioning in various areas of life, such as relationships, work, ability to care for oneself, and the symptoms must not be related to outside influences, such as drug or alcohol use, or the underlying medical diagnosis. For example, if a person has a brain tumor in a part of their brain that changes their emotions or reactions to events, that would not be considered PTSD. Drug or alcohol use does not mean that a person doesn’t have a diagnosis of PTSD. The important thing is making sure the symptoms started before the drug or alcohol use, or continued after stopping it. It is common for people who experience PTSD to self medicate with prescription medication, non-prescription drugs, or alcohol.
In many ways, PTSD shows the same signs of trauma that are discussed above: Hypervigilance, minimization, or out of proportion emotional reactions. Other signs include dissociation from our body or unexplained physiological reactions like hives or panic attacks.
Looking at our sleep can be a helpful way to spot PTSD specifically. It might be PTSD if there are troubles with "busy brain" when quieting our mind for bed, or if we are dependent on the sound of radio or TV to fall asleep. Along these lines, another hint could be if we experience frequent "twilight jerks" due to nightmares.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders, 5th Edition. DSM-5.
We know traumatic events are when something happened, and traumatic reactions are how we respond later on over time. What is important to realize is that not all traumatic events lead to ongoing traumatic reactions.
In fact, the first triggering event is usually easy to handle. We can frame an event to its specifics. We carry that traumatic event with us and often forget about it until something reminds us of it.
Anything can remind us of a traumatic event - a sound, feeling, or smell - and when we experience that sensation, it can send us reeling back to the first traumatic event. We start to notice our ongoing traumatic reactions to triggers when those sensations continually cause us to feel like the traumatic event is happening all over again.
How does Covid-19 affect trauma?
This is a widespread traumatic event. For some it’s their first experience with medical trauma, but for many others this is a reawakening. If you have difficulty breathing, a compromised immune system, or need routine testing - Covid-19 is providing a second traumatic event that becomes increasingly hard to ignore. To a certain extent - everyone is dealing with the aftermath and trauma that Covid-19 has caused.
If it feels like we all have trauma - you’re right! The world has been rapidly changing since 2020, and there is widespread trauma that feels overwhelming.
So what can we do about it? The first step is engaging and understanding your own trauma, and you’re already here. Let’s take another deep breath here, and look at practices to help cope.
If it feels like we all have trauma - you’re right! The world has been rapidly changing since 2020, and there is widespread trauma that feels overwhelming.
So what can we do about it? The first step is engaging and understanding your own trauma, and you’re already here. Let’s take another deep breath here, then let's learn more about practices to help cope with trauma.